History of the SDI Initiative
- The SDI program began in 2008, through collaboration between the World Bank Group and African Economic Research Consortium and was supported by the Hewlett Foundation and the African Development Bank. As a direct response to the canonical World Development Report 2004: Making Services Work for Poor People, the SDI initiative laid the groundwork for the innovative way of measuring the quality of health and education at the point where the service meets the citizen.
- The first SDI surveys were developed and piloted in 2010. The surveys introduced novel methodologies in measurement of quality of public service provision including innovations in assessing provider competency and measurement of absenteeism in health facilities. The first full SDI survey was completed in 2012 and quickly ramped up in the Africa region.
- Between 2012 and 2018, almost a dozen surveys were completed in the Africa region, and the surveys focused on maternal and child health, communicable diseases, inputs and infrastructure.
- 2018 marked a watershed moment in global health with the introduction of three global reports that emphasized the importance of improving quality of care in health care facilities to realize the Sustainable Development Goals (SDGs). The SDI Health Survey Team undertook a comprehensive revamp (described below) to ensure that the survey tools responded to the latest.
SDI Health Survey Revamp: Assessment Methods
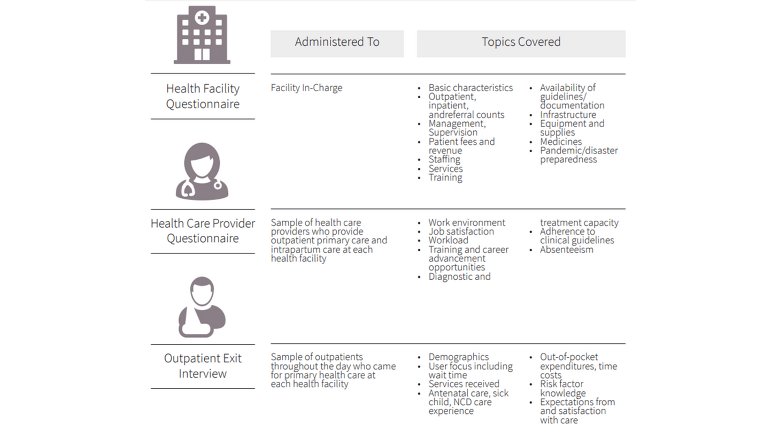
SDI Health Surveys are in-person, facility-based surveys with questionnaires capturing health facility characteristics, health care provider information, and patient experience. The survey takes place over the course of two days (one pre-announced facility visit and one unannounced surprise facility visit) and is typically administered by field teams of 2-6 enumerators depending on the size of the facility.
Three questionnaires were developed, each distinguished by who the intended respondent was –facility manager, health care providers, patients –for clarity and ease of administration. The domains and subdomains in the framework are covered across the three questionnaires.