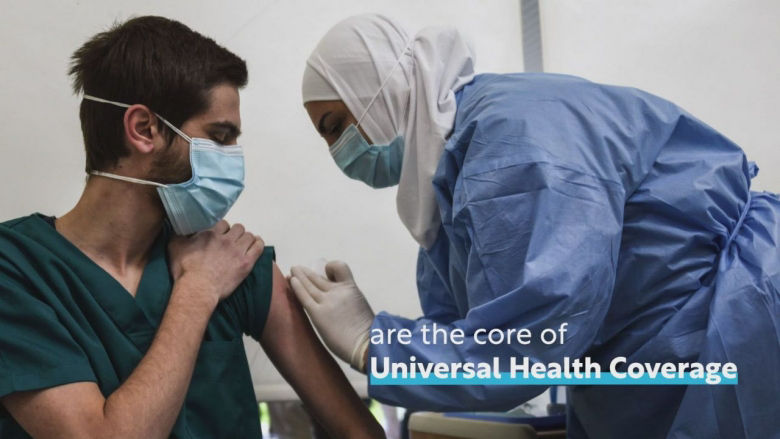
Universal health coverage (UHC) is about ensuring that everyone, especially the most vulnerable, has access to the quality health care they need without suffering financial hardship. It is key to achieving the World Bank Group’s mission to end extreme poverty and boost prosperity on a livable planet, and it is the driving force behind all of the Bank’s health and nutrition investments.
Investing in health is one of the most powerful drivers of economic growth and job creation. As the World Bank Group works toward its ambitious goal of supporting countries to expand health services to 1.5 billion people by 2030, the impact extends well beyond improving care – it strengthens human capital, fuels economies, and creates millions of jobs. Healthy populations are more productive, resilient, and capable of contributing to economic development in their countries.

Slowing progress towards UHC
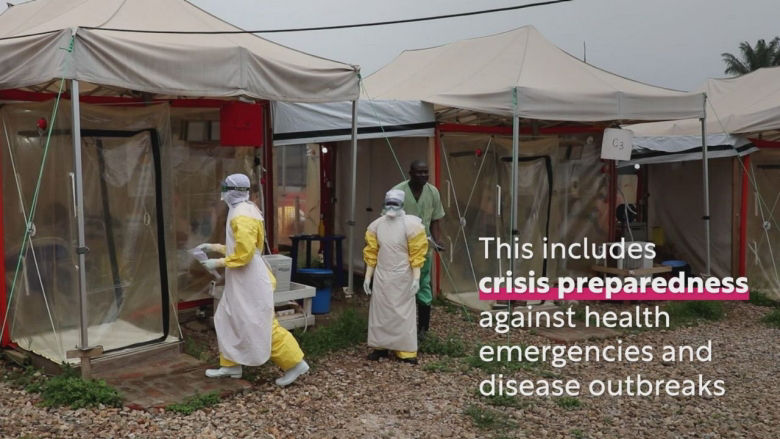
Since 2015, health service coverage has stagnated and financial hardship due to out-of-pocket health spending has worsened, undermining efforts to eradicate poverty globally.
Half of the world’s population -or 4.5 billion people- is not covered by essential health services, and 2 billion people face severe financial hardship |
Over the past two decades, less than a third of countries have improved health service coverage and reduced catastrophic out-of-pocket health spending. Moreover, most countries for which data are available are off-track in either service coverage, financial protection, or both. Read the latest UHC Global Monitoring Report.
To reach the goal of UHC, substantial public sector investment and accelerated action by governments and development partners are essential. Key actions include a radical reorientation of health systems towards a primary health care approach, advancing equity in health-care access and financial protection, and investing in robust health information systems.
Global commitments for women, children and adolescents are falling behind.

The world has made remarkable progress in reducing child mortality, and the mortality of children under five years of age has fallen by 52% since 2000. Thanks to life-saving interventions and better access to health services, millions of children have survived and thrive. This reflects decades of investment and collaboration by governments, communities and partners. Millions of children have survived thanks to life-saving interventions. Yet, latest estimates show that progress is slowing – and that millions of children are still dying from preventable causes. In 2023, an estimated 4.8 million children died before the age of five, including 2.3 million newborns.
Similarly, latest data show a 40% global decline in maternal deaths between 2000 and 2023 – largely due to improved access to essential health services. But the pace of improvement has slowed significantly since 2016, and an estimated 260 000 women died in 2023 as a result of complications from pregnancy or childbirth – about one mother dying every two minutes.
Health systems will be increasingly affected by aging populations
The world’s population has been aging at a dramatic speed and many countries are ill-prepared to address the magnitude and pace of demographic shifts. By 2050 at least one third of the world population will be over 60 years of age and countries need to adjust to the opportunities and challenges this rapid demographic transition presents.
The impact of aging populations will ripple through labor markets and social policies. To navigate this evolving landscape, investing in the health and wellbeing of the working-age population is imperative. In low- and middle-income countries, non-communicable diseases already account for over 70% of all deaths, and a significant portion of disease and disability.
The World Bank is promoting healthy, productive, and inclusive longevity which requires action throughout a person’s life. Most important is the timely and effective prevention and control of non-communicable diseases such as diabetes, respiratory diseases, heart diseases, cancers and depression.
Climate change is also a critical contributor to the burden of NCDs through factors such as air pollution, heat stress, and extreme weather events.
These shifts require health systems to adapt to be more responsive to changing needs of the population, but such changes also have implications for the financing of health systems.
Health is an investment, not an expense
Last Updated: Jul 10, 2025