Lakshmi Perera, a 48-year-old woman from Kalutaram, Sri Lanka had trouble losing weight. She started going to a healthy life center the government set up to beat the growing rates of non-communicable diseases in the country. Her life has transformed ever since.
“They taught us how to eat healthy and how to stay fit, but it was not always easy to do,” Perera said. “Now, I have joined an exercise class and within six months I lost 10 kilos.”
In Sri Lanka—the fastest ageing population in South Asia—the country is facing a population over 60 that is expected to double in the next 25 years. With the support from the World Bank, the government has established Healthy Life Centers to help prevent, detect, and treat non-communicable diseases at the community and primary healthcare levels. The Centers target vulnerable poor populations, men and women over 40 years old, and teach at them about the risk of NCDs and how to prevent, detect and manage them to be able to live healthier and more fulfilling lives.
“I get the push I need, I can feel firsthand the benefits of losing weight, and I am more motivated than ever to continue my weight loss journey,” said Perera.
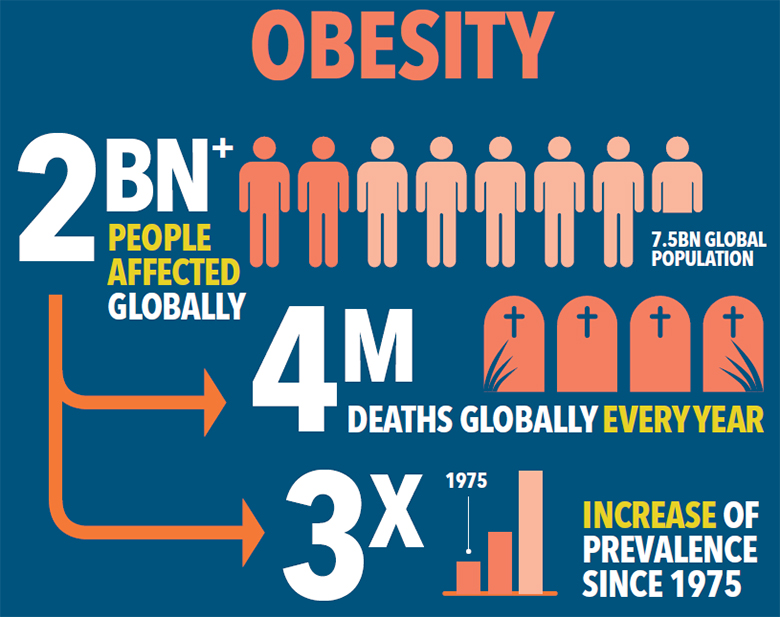
Despite increases in life expectancy, the rise in chronic and non-communicable diseases have become a global threat.
Chronic and non-communicable diseases have become a growing concern in all countries irrespective of income level.
“One of the most effective ways to address non-communicable diseases is by ramping up investments in affordable, quality primary health care”, says Dr. Muhammad Pate, Global Director for Health, Nutrition and Population at the World Bank. “This makes sense both from a health and an economic perspective. Putting more resources on the frontlines to detect and treat conditions early, before they become more serious, saves lives, improves health outcomes, reduces health care costs and strengthens outbreak preparedness.”